Predicting leukemia in myelodysplastic syndromes
A new molecular score can identify patients with myelodysplastic syndromes that are at higher risk of developing leukemia, based on their genetic profile. A step forward for precision medicine
What is the probability that a patient with myelodysplastic syndrome will develop leukemia over time? According to the results of a new study and thanks to the advancement of genomics and artificial intelligence, we can now answer this question with increased precision. The study – coordinated by Matteo Della Porta, full professor of Hematology at Humanitas University and clinical group leader at Humanitas Research Hospital – was published in the Journal of Clinical Oncology and demonstrated the accuracy of a new score, called IPSS-M, in predicting leukemic evolution and life expectancy in patients with myelodysplastic syndromes. The new score is computed using genomic data from patients’ neoplastic cells.
The study was conducted within the Horizon2020 project GenoMed4All and in collaboration with Gastone Castellani, from the University of Bologna. It was made thanks to the support of EuroBloodNET, the European reference network for rare hematological diseases, and AIRC Foundation for Cancer Research.
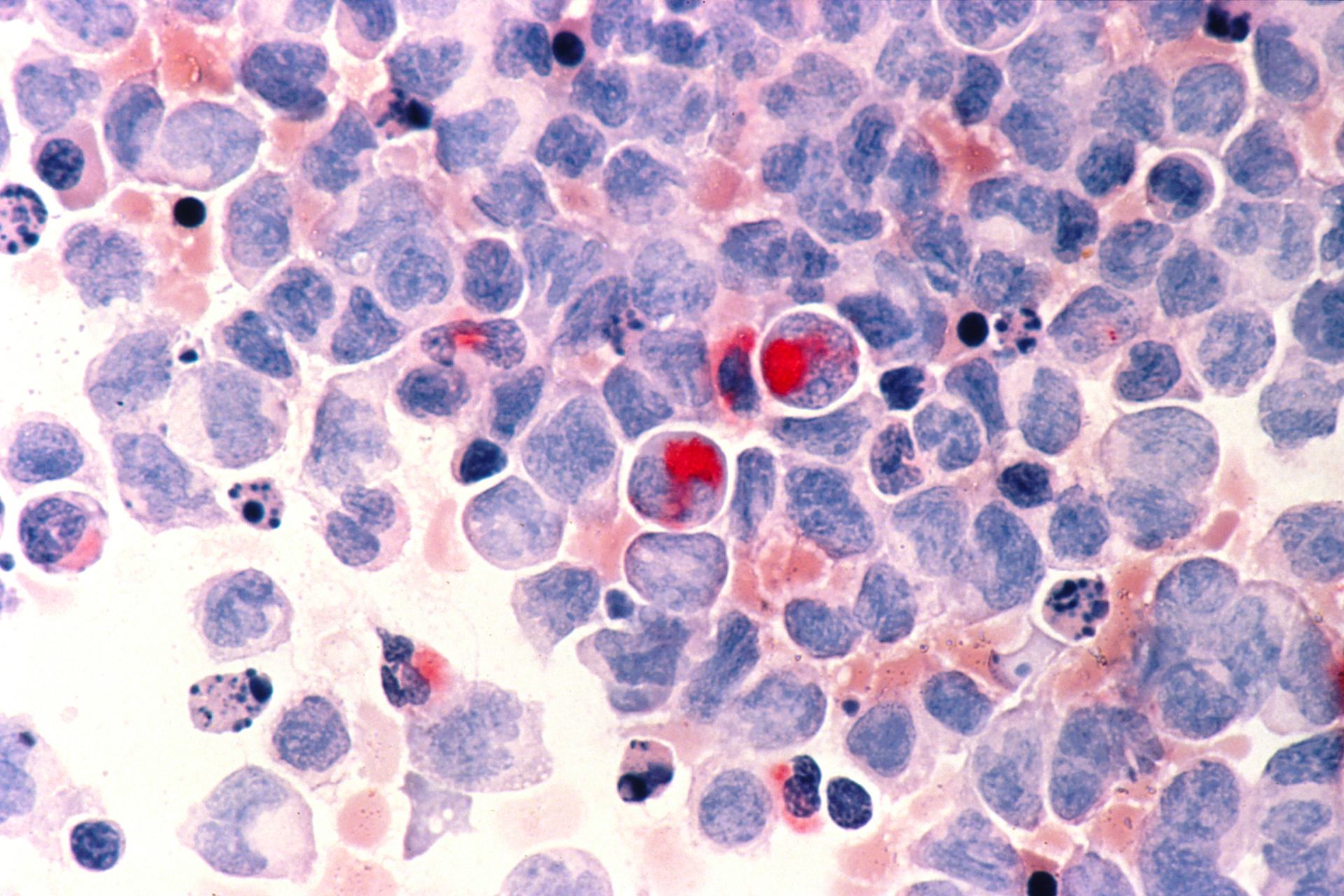
What are myelodysplastic syndromes
Myelodysplastic syndromes (MDS) are heterogeneous neoplasms that vary widely from patient to patient, ranging from indolent, slowly progressing neoplasms to aggressive forms that rapidly evolve into acute myeloid leukemia. MDS arise most frequently in adults and elderly people. A bone marrow transplant, also known as a stem cell transplant, is the only treatment option that can potentially cure a myelodysplastic syndrome, but it is a procedure that present major critical issues. About 3,000 new cases of myelodysplastic syndrome are diagnosed each year in Italy alone.
Given the widely diverse manifestations of MDS and the fact that the syndrome not always requires an immediate intervention, hematologists decide the best treatment strategy for each patient based on a risk assessment. To do it, they usually compute a score called IPSS-R, which is based on clinical indicators such as the number of leukemic cells in the bone marrow, the levels of white, red and platelet cells in the blood (cytopenias) and chromosomal aberrations in hematopoietic cells (cytogenetic abnormalities). The score does not take into account any genomic information regarding the syndrome, even though we know that mutations in specific genes can influence MDS progression.
A new molecular score for MDS syndromes
The new score, called IPSS-M, was developed thanks to the advancement in the genomics of myelodysplastic syndromes, a field in which prof. Matteo Della Porta has made seminal contributions in the past decade. The score is based on the identification, in patients’ blood samples, of specific pathogenic variants of 31 genes associated with MDS progression and has been tested on 2.876 patients with myelodysplastic syndromes.
“The results demonstrated that IPSS-M significantly improves our ability to predict, for each patient, the risk of leukemic evolution and life expectancy. Moreover, the new score provides clinicians with an accurate and validated tool to identify the patients who are the best candidates for hematopoietic stem cell transplantation and the optimal time at which to perform the procedure,” explains prof. Della Porta. “The use of high-precision predictive tools is also an important aid for patients, because it helps them face difficult therapeutic choices with greater awareness and peace of mind.”
Since molecular testing is not yet routine in every hospital and although the best predictive power is achieved by analyzing all the 31 genes, researchers have identified a smaller group of 15 genes to facilitate the clinical implementation of a simplified version of the IPSS-M score.
“The development of innovative methods to analyze big data has made it possible to shorten the time with which biomedical research results – such as the identification of mutations that drive disease progression – can be translated into clinical practice, improving patients’ life,” says Elisabetta Sauta, data scientist at the Humanitas AI Center. “This achievement was possible thanks to the multidisciplinary collaboration between clinicians, researchers and data scientists: only by combining different perspectives and methods we can improve our understanding of highly complex, rare and heterogeneous diseases, such as MDS syndromes.”