Leukemias: new score helps identify the right time for bone marrow transplant
A team of doctors, researchers and data scientists has validated an innovative assessment tool, the molecular IPSS score, to identify patients with myelodysplastic syndromes at higher risk of leukemia and predict the optimal timing for hematopoietic stem cell transplantation
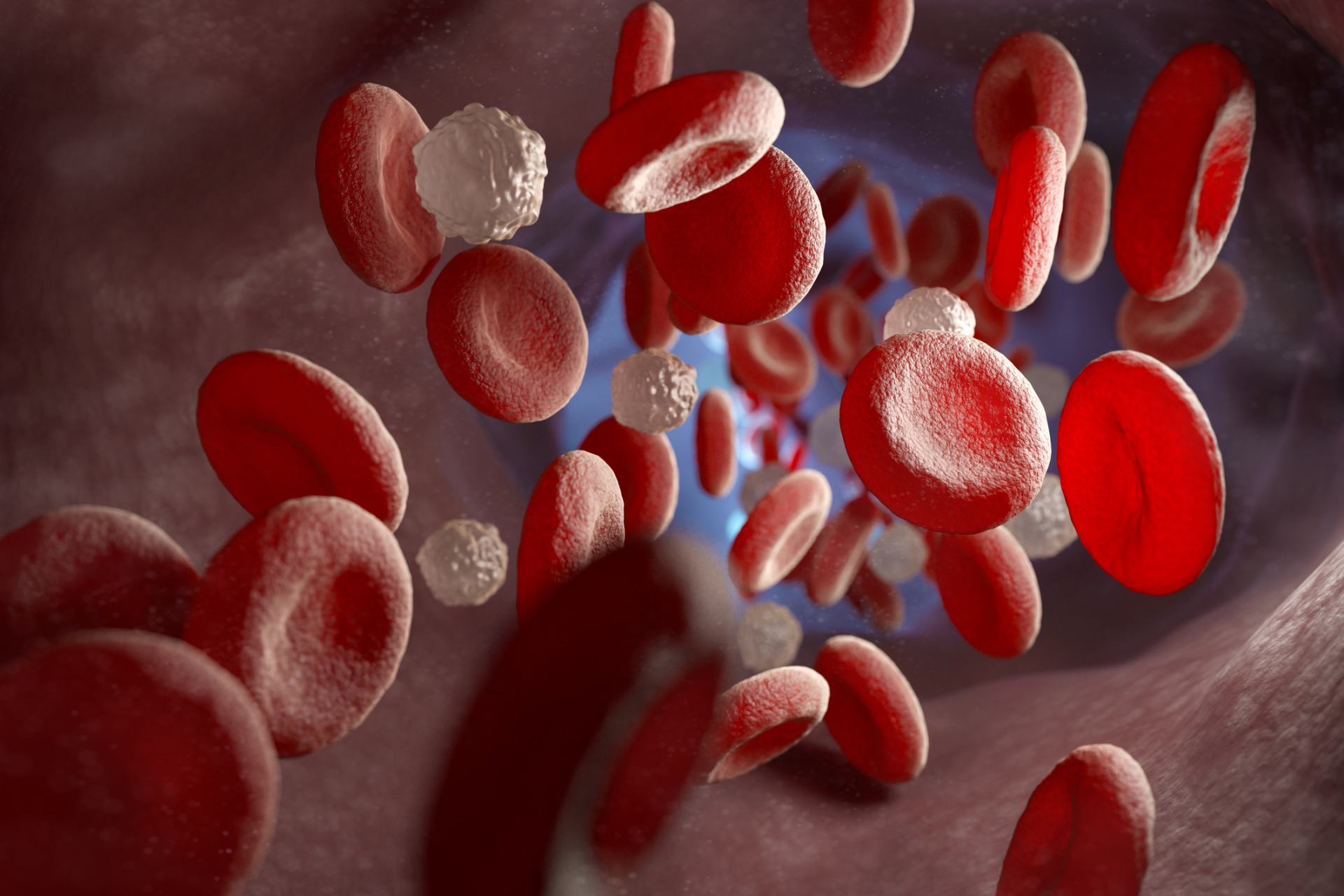
Donor bone marrow transplantation is the only potentially effective therapy for patients with myelodysplastic syndromes – a group of blood proliferative diseases that may stay indolent for years or rapidly progress to acute myeloid leukemia. Understanding which patients are at higher risk of progression and when is the best time to perform the transplant is crucial.
In a study published in the Journal of Clinical Oncology, an international group of researchers led by Prof. Matteo Della Porta – Clinical Group Leader in Humanitas and full professor of Hematology at Humanitas University – demonstrated the predictive effectiveness of a new risk score called “IPSS-M,” which includes tumor genetic characteristics.
“Compared to the prognostic indicators in use today, IPSS-M predict disease progression in patients more accurately and can suggest the best time for transplantation. This is an important step towards personalized medicine, based not only on the patient’s clinical and demographic characteristics but also on the molecular and genetic features of the disease,” says Prof. Della Porta.
The study was made possible by the funding of two European projects – GenoMed4All and Synthema – which include among the Italian partners also the University of Bologna and Politecnico di Milano, with the further support of the AIRC Foundation for Cancer Research.
Myelodysplastic syndromes and prognostic markers
With over 3000 diagnoses per year in Italy alone, myelodysplastic syndromes are blood disorders that occur more frequently in the elderly. The only potentially curative therapy is hematopoietic stem cell transplantation, a procedure that presents significant risks and challenges, especially in advanced age.
Today, hematologists decide on treatment strategies, including the opportunity and timing of donor transplantation, based on a clinical score called IPSS-R, which is calculated from values such as the number of leukemic cells in the bone marrow, levels of white blood cells, red blood cells, and platelets in the blood, as well as the presence of abnormalities in the chromosomes of blood cells. However, this indicator does not contain information about the genomic profile of the syndrome – i.e., about the presence of specific genetic mutations in tumor cells – which we now know to be crucial for disease progression and therefore for the effectiveness of treatments.
A new score to advance precision medicine
In 2023 the same group of researchers demonstrated that a new molecular score called IPSS-M – based also on mutations in 31 genes – improves the prediction of leukemic evolution risk and patients’ life expectancy.
Now, thanks to the retrospective analysis of a population of over 7000 patients with myelodysplastic syndromes from 26 hospitals across Europe and the United States, researchers have taken another step forward: they have demonstrated that the use of the new molecular score IPSS-M – compared to the one used in clinical practice, IPSS-R – would change therapeutic choices in 17% of cases, modifying the timing of bone marrow transplantation. Specifically: 15% of patients who would currently undergo immediate transplantation would benefit, according to IPSS-M, from a delay in the procedure, while 19% of those whose transplantation would normally be delayed would instead benefit from immediate intervention.
Della Porta explains: “This happens because some genetic mutations in the tumor provide key information about the actual risk of disease progression, as well as the likelihood of relapse: taking into account these mutations allows us to refine clinical evaluation, increasing the risk profile in some patients and reducing it in others, with the same clinical indicators.”
Although there are still many hospitals that cannot perform routine molecular and genomic tests, the costs of analyses are decreasing, and the technologies necessary for these tests are becoming increasingly accessible. That’s why the transition to a molecular approach is now closer than ever: to further facilitate the implementation of the new score in the real world, the group of researchers has reduced the number of key genes to be analyzed to 15.
“The result achieved was only possible thanks to the collaboration between doctors, data scientists, and experts in artificial intelligence, and the access to thousands of data shared within the consortium of the European project GenoMed4All. A good example of what can be done to improve care by collaborating internationally and bringing together different approches and skills,” concludes Della Porta.