The immune system orchestrates neurodevelopment in the hippocampus
The study opens a new chapter in the field of neuroimmunology, with implications for neurodevelopmental and neurodegenerative diseases, especially Alzheimer’s
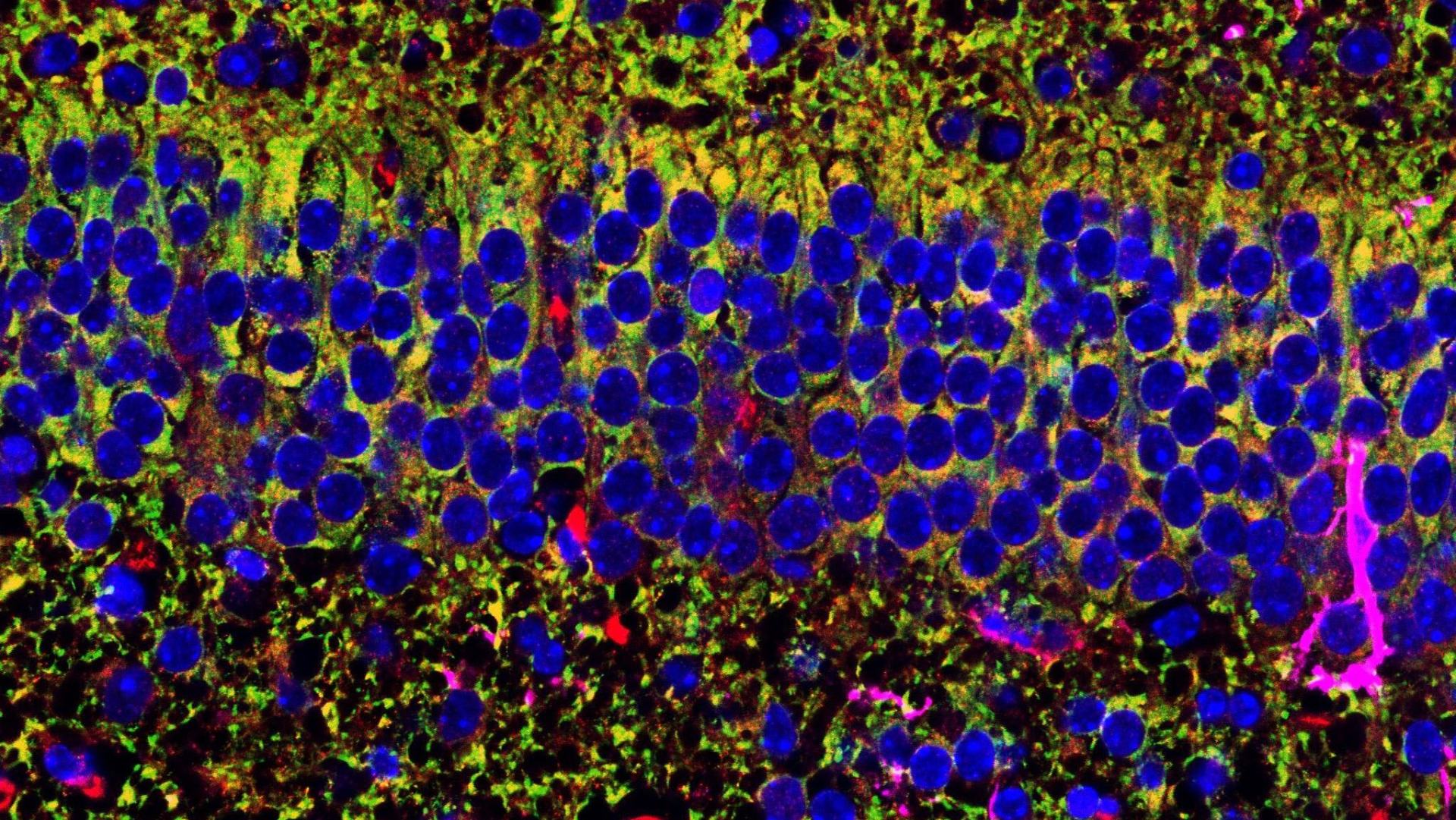
The immune system does not merely protect the brain from injuries or infections; on the contrary, recent research in the neuroscience field has shown that immune system plays a crucial role in controlling brain homeostasis and function throughout our life. According to a study published today in Immunity, the immune cells residing in the brain, known as microglial cells, control the development and maturation of neurons in the hippocampus, the area responsible for memory. They accomplish this by shaping the metabolism of neurons composing this area through a receptor called TREM2.
The study, led by Michela Matteoli, full professor of Pharmacology at Humanitas University and director of the Neuroscience Program at Humanitas Research Hospital, adds an important piece to the puzzle concerning the complex relationship between the immune and the nervous system, a piece that could change our view of various neurodevelopmental and neurodegenerative diseases, including Alzheimer’s.
“We have discovered that when the microglial receptor TREM2 does not function properly, memory neurons in the hippocampus show abnormalities in their bioenergetics during development, with long-lasting implications in the adulthood,” explains Prof. Michela Matteoli.
“The discovery is very exciting, not only as it unveils a novel function of microglial cells in controlling neuronal development but also because it is known that defects in neuronal metabolism in this area occur in various neurodegenerative diseases, including Alzheimer Disease (AD). Moreover, the recent evidence that mutations in TREM2 gene constitute a risk factor for the onset of AD, as demonstrated by the genetic screening studies on patients, suggests the relevance of the mechanism discovered”.
The study was conducted in collaboration with the group led by Simona Lodato, group leader and associate professor at Humanitas University, Katia Cortese from the University of Genoa, and Rafael Arguello from CNRS in Marseille. Among the funding sources that made this project possible, were the prestigious ERC Advanced Grant obtained by Matteoli in 2022 and a postdoc fellowship from the High Postodoctoral Profile (HiPPO) program from Fondazione Humanitas per la Ricerca, which supported the work of Erica Tagliatti, the first author of the study together with Genni Desiato.

The Continuous Dialogue Between Immunity and the Brain: The Role of TREM2
In recent years, the concept of the brain as an immunologically privileged organ, isolated from the rest of the body, has been revolutionized. Thanks to the scientific research, we now know that since the early stages of development till aging, the ongoing dialogue between neuronal cells and immune cells ensures the brain’s proper functioning, while its disruptions may result in multiple diseases.
Central to this continuous interplay are microglial cells – the immune cells residing in the brain – and particularly their receptor named TREM2, known in the field of neuroscience already in 2013 because its mutations were associated with an increased risk of dementia and AD.
The mechanism that links faulty versions of TREM2 and AD onset is investigated since. It could pave the way for new therapeutic approaches for AD, which currently lacks effective treatments. The research published in Immunity, although limited to preclinical studies, gives a significant contribution to the filed as it reveals a novel role of TREM2 in the formation and function of memory-related areas, which are preferentially affected in Alzheimer’s disease.
The Discovery: TREM2 Modulates Metabolism in Hippocampus Memory Area
“According to the results obtained in this work, in the absence of TREM2, neurons that make up the memory area in the hippocampus, namely the CA1 region, show up a developmental delay which is accompanied by transcriptional and behavioral abnormalities – especially of metabolic nature – that persist over time. Their mitochondria – which represent the ‘power-stations’ of the cells – are fewer in number and have a reduced structure and function,” explain the study’s first authors, Erica Tagliatti and Genni Desiato. “For the first time, we have demonstrated that microglial cells and their receptor TREM2 play a role in controlling the maturation of memory neurons and, in particular, their metabolic profile.”
The discovery was conducted in the laboratory and on preclinical models. Further research will be necessary to understand its real implications in the study of diseases such as dementia and AD, but many avenues have opened up. Patients with genetic variants of TREM2 may indeed have metabolic defects – so far ignored – in the area of the brain responsible for memory formation, alterations that could weaken this region and make it more susceptible to the onset of AD. Furthermore, the metabolic impact due to the lack of TREM2 during early development, as observed by the researchers, could even reoccur later in life, when we know that TREM2 receptor levels naturally decrease.
“This research demonstrates once again that in the brain development and aging are two sides of the same coin and should be studied in conjunction. In the last years, recent discoveries have shown that certain molecules, historically associated with neurodegenerative diseases, play important roles in brain development. Indeed, functional alterations of these proteins during brain formation can lead to long-lasting detrimental effects. This is particularly relevant for the brain, as this tissue that does not undergo the continuous cellular renewal observed in other organs of the body,” concludes Michela Matteoli.