Postbiotics released by gut microbiota improves cancer immunotherapy
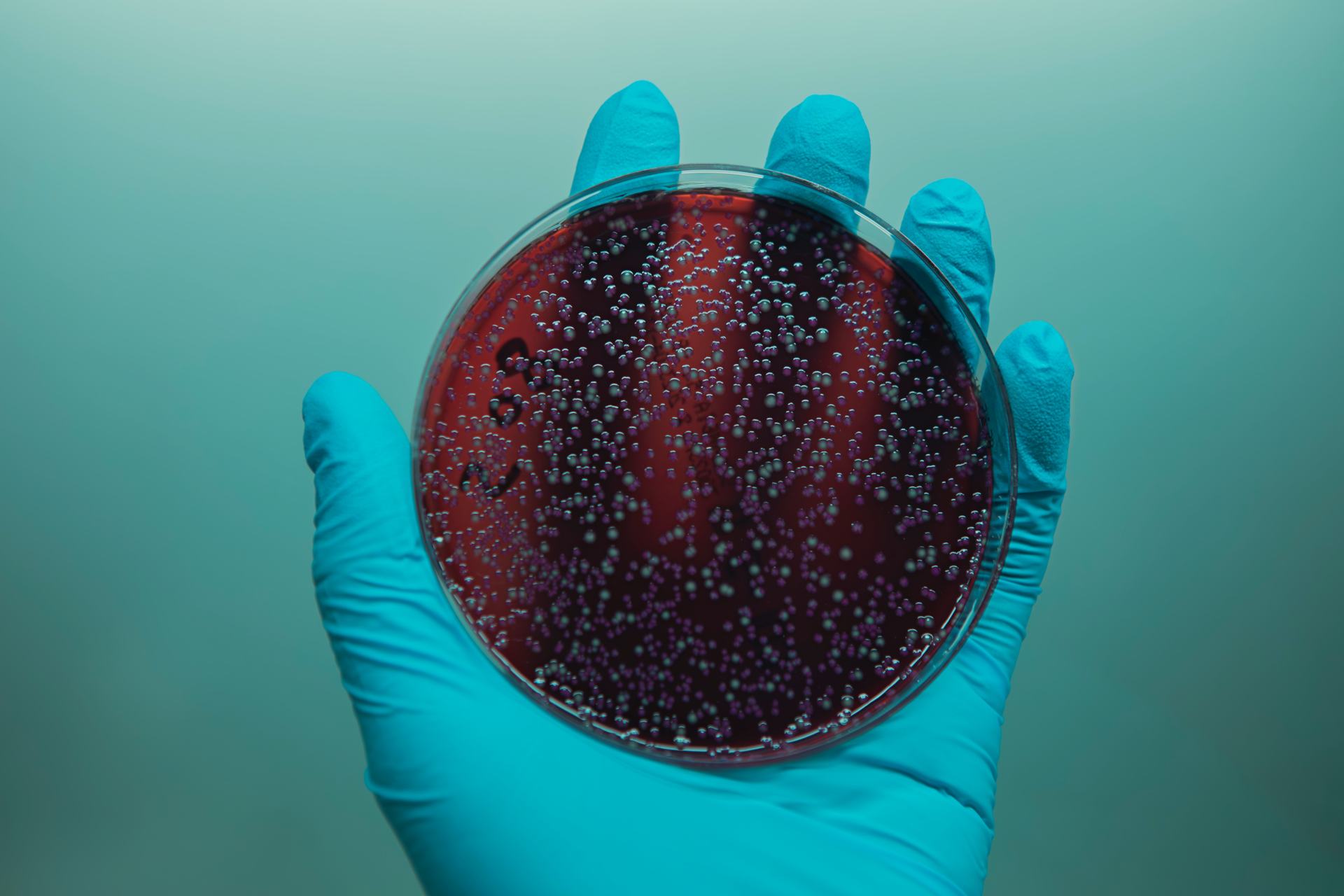
Humanitas researchers have identified a strain of bacteria whose metabolic outputs make cancer cells more visible to the immune system, enhancing the efficacy of immunotherapies
From microbiota research comes new hope for improving the efficacy of immunotherapies. According to the results of a study led by Prof. Maria Rescigno, head of the Laboratory of Mucosal Immunology and Microbiota at Humanitas Research Hospital and Vice Director for Research at Humanitas University, a particular strain of gut bacteria is able to enhance the efficacy of these drugs. The data obtained are published in the journal Cancer Cell.
The effectiveness of immunotherapy is limited by the immune system’s ability to recognize tumor cells: although these drugs make T lymphocytes more prone to attack the tumor, their effect can be reduced, or even nullified, if the tumor cells are able to hide, by suppressing the membrane receptors used to identify them.
“In our study, we show that Lactobacillus paracasei, one of the bacterial strains of the intestinal microbiota, induces cancer cells to show their receptors and thus become ‘visible’ again to the immune system. The mechanism is mediated by postbiotics, metabolic substances produced by bacteria,” explains Prof. Rescigno. The researchers have also shown in different experimental models of cancer that, when administered together with immune check-point inhibitors, such postbiotics improve the drugs’ efficacy.
The study – although still limited to in-vivo and in-vitro experiments – paves the way for new therapeutic approaches based on the combination of immunotherapy drugs already approved in the clinic and postbiotics, and was made possible thanks to the support of AIRC Foundation for Cancer Research and of the Alan Ghitis Association.
The influence of microbiota on patients’ response to cancer therapies
Recent studies have highlighted the ability of the gut microbiota to influence the response to cancer therapies, especially immunotherapies. In the case of melanoma and other cancers of epithelial origin, for example, it has been shown that harboring certain bacterial strains in the gut is what distinguishes patients who respond positively to immune checkpoint inhibitors from those who do not benefit from the treatment.
But why? And how can this knowledge be harnessed to enhance cancer therapies and increase the number of patients who can benefit from them? To find an answer, the group led by Maria Rescigno focused on the molecules produced by bacteria – the so-called postbiotics.
“The interest in postbiotics is due to two fundamental aspects,” explains Maria Rescigno. “The first is their ability to affect the whole body, mediating the remote action of gut microbiota in other organs: in fact, these molecules easily cross the gut vascular barrier and enter the bloodstream, reaching the site of the tumor; the second is that they constitute a very powerful and precise therapeutic tool: instead of transplanting or modifying the microbiota – as it is done in some early clinical studies – we could act downstream, directly administering only the beneficial molecules produced by it.”
Postbiotics that unmask cancer cells
The bacterial strain identified by Humanitas researchers it’s called Lactobacillus paracasei and it is already known for its anti-inflammatory properties. According to the study published today in Cancer Cell, postbiotics produced by this strain are able to unmask cancer cells because they force them to show HLA receptors, the ones used by T lymphocytes to assess their nature.
“The loss of HLA receptors is a well-known immune evasion mechanism, described in many types of cancer, such as melanoma, breast, colorectal, lung and bladder cancer” explains Valentina Ferrari – now at IRB in Bellinzona and first author of the study – whose work was supported by a fellowship of the Alan Ghitis Foundation.
However, this is the first time we demonstrate the ability of postbiotics to affect HLA expression on tumor cells and thus their ability to make the tumor more easily visible to T lymphocytes. The researchers have also shown in experimental models of colorectal cancer and breast cancer that by adding these specific postbiotics to immune checkpoint inhibitors the drugs can better control tumor growth.
“Although the suppression of HLA receptors in tumors has been observed and studied for decades, a safe and effective remedy has never been found before. That’s why the results obtained are so relevant, even if they came from experimental models of cancer,” says Prof. Rescigno. “The next step will be to conduct a clinical trial to test whether the approach really constitutes a new and effective strategy for patients who do not respond to immunotherapies.”